THE IMPACT OF CLIMATE CHANGE ON ZOONOTIC DISEASE TRANSMISSION
Zoonotic diseases, which are transmitted between animals and humans, represent a significant public health challenge. These diseases account for nearly 60% of emerging infectious diseases, with approximately 70% originating from wildlife. Climate change exacerbates the risk and spread of zoonotic diseases through changes in temperature, precipitation, and extreme weather events (Ahmed et al., 2019). The increasing influence of climate change on zoonotic diseases necessitates an integrated and collaborative approach to mitigate its effects on global health systems.
Climate Change and Disease Transmission
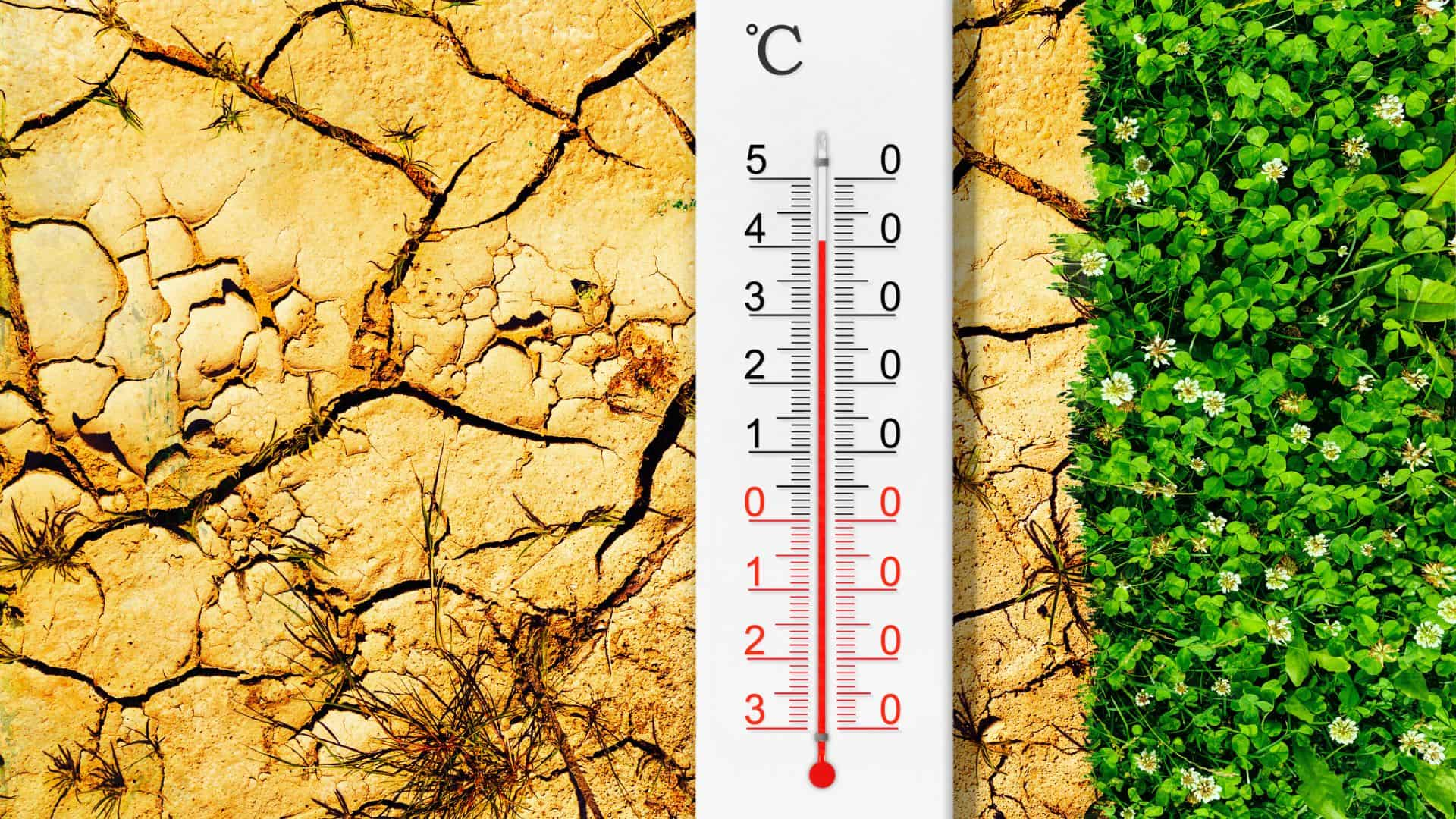
Climate change significantly impacts the ecological balance of vectors, pathogens, and hosts. Rising temperatures enhance the reproduction, survival, and activity of vectors like mosquitoes, ticks, and fleas, thereby increasing the likelihood of disease transmission (Liu-Helmersson et al., 2014). Similarly, shifts in precipitation patterns also influence the spread of zoonoses. Excessive rainfall can create stagnant water, ideal breeding sites for disease-carrying vectors such as mosquitoes. Conversely, droughts force communities to store water in containers, which often become breeding grounds (Ahmed et al., 2019). Regions that previously experienced minimal vector-borne disease risks, such as parts of Europe, now face increased threats due to warming climates and extreme weather (Åström et al., 2012).
Case Study: Dengue Fever
Dengue fever is a mosquito-borne viral disease that exemplifies how climate change influences zoonoses. Annually, about 390 million people are infected with dengue, and the disease burden is expected to increase with changing climate conditions (Colón-González et al., 2013). Aedes aegypti mosquitoes, which transmit dengue fever, thrive between 20°C and 32°C (Chandrashekar, 2023). Warmer temperatures shorten mosquito life cycles and hasten viral replication, making outbreaks more frequent and severe. Additionally, urbanization and poor waste management provide mosquito breeding habitats, worsening transmission risks in densely populated areas (Xu et al., 2024).
Extreme weather events such as floods exacerbate the situation. Floodwaters create temporary mosquito breeding sites, while damaged infrastructure hampers effective disease control. Despite these challenges, temperatures above 32°C can suppress mosquito survival, showcasing the complex relationship between climate variables and vector-borne diseases (Ahmed et al., 2019).
Habitat Disruption and Zoonotic Spillovers
Human activities like deforestation and habitat destruction also amplify zoonotic disease risks. When natural ecosystems are disrupted, humans come into closer contact with wildlife, increasing the likelihood of zoonotic spillovers. For instance, deforestation has been linked to outbreaks of diseases such as the Nipah virus and Ebola, where habitat destruction forces wildlife closer to human populations (Rocklöv and Dubrow, 2020). This disruption undermines the natural ecological barriers that previously minimized human exposure to wildlife pathogens.
Strategies for Mitigation and Adaptation
Mitigating the impact of climate change on zoonotic diseases requires comprehensive and multi-sectoral strategies. Integrated Vector Management (IVM) combines biological, chemical, and community-based approaches to control vector populations effectively (Ahmed et al., 2019). For example, larvicide use and habitat destruction can limit mosquito breeding, while public awareness campaigns educate communities about preventive measures (Campbell-Lendrum et al., 2015).
Urban planning also plays a critical role. Incorporating green infrastructure, proper drainage systems, and sustainable waste management into urban designs can reduce vector habitats (Xu et al., 2024). These measures are essential in densely populated areas, where rapid urbanization often outpaces infrastructure development.
Early disease detection and surveillance systems are vital for timely intervention. Predictive models that integrate climate and epidemiological data enable governments and public health agencies to anticipate outbreaks and allocate resources efficiently (Liu-Helmersson et al., 2014). Advanced diagnostic tools and robust reporting systems further improve response times and reduce disease burdens (Rocklöv and Dubrow, 2020).
The One Health Approach
A holistic approach, such as One Health, integrates human, animal, and environmental health to address zoonotic diseases comprehensively. One Health emphasizes interdisciplinary collaboration, ensuring that policies consider the interconnectedness of ecosystems, public health, and climate change (Rupasinghe et al., 2022). For instance, joint efforts among veterinarians, environmentalists, and medical professionals can enhance surveillance, prevent zoonotic spillovers, and mitigate the effects of climate change on disease transmission.
Building Resilience for the Future
Climate change will continue to influence zoonotic disease dynamics, making resilience-building a priority. Strengthening international cooperation, enhancing public health infrastructure, and investing in research are crucial to addressing future challenges. Public engagement is also critical, as informed communities are better equipped to adopt preventive practices and contribute to vector control initiatives (Campbell-Lendrum et al., 2015).
The global community can reduce the burden of zoonotic diseases through targeted interventions, innovative technologies, and interdisciplinary collaboration. Mitigating climate change’s effects on health systems is essential for ensuring the well-being of future generations and achieving sustainable development goals.
References
- Ahmed T, Hyder MZ, Liaqat I, Scholz M. Climatic conditions: conventional and nanotechnology-based methods for the control of mosquito vectors causing human health issues. International journal of environmental research and public health. 2019 Sep;16(17):3165.
- Åström C, Rocklöv J, Hales S, Béguin A, Louis V, Sauerborn R. Potential distribution of dengue fever under scenarios of climate change and economic development. Ecohealth. 2012 Dec;9:448-54
- Campbell-Lendrum D, Manga L, Bagayoko M, Sommerfeld J. Climate change and vector-borne diseases: what are the implications for public health research and policy?. Philosophical Transactions of the Royal Society B: Biological Sciences. 2015 Apr 5;370(1665):20130552.
- Chandrashekar V. As Temperatures Rise, Dengue Fever Spreads and Cases Rise. Yale Environment 360. Available from: https://e360.yale.edu/features/dengue-fever-climate-change
- Colón-González FJ, Fezzi C, Lake IR, Hunter PR. The effects of weather and climate change on dengue. PLoS neglected tropical diseases. 2013 Nov 14;7(11):e2503.
- Liu-Helmersson J, Stenlund H, Wilder-Smith A, Rocklöv J. Vectorial capacity of Aedes aegypti: effects of temperature and implications for global dengue epidemic potential. PloS one. 2014 Mar 6;9(3):e89783.
- Rocklöv J, Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nature immunology. 2020 May;21(5):479-83.
- Rupasinghe R, Chomel BB, Martínez-López B. Climate change and zoonoses: A review of the current status, knowledge gaps, and future trends. Acta Tropica. 2022 Feb 1;226:106225.
- Xu C, Xu J, Wang L. Long-term effects of climate factors on dengue fever over a 40-year period. BMC Public Health. 2024 May 30;24(1):1451.
Author

Ibeh Esther Nmasichukwu
Ibeh Esther Nmasichukwu is a 600-level veterinary medicine student at the University of Nigeria, Nsukka, and the Chair of IVSA Nigeria’s Standing Committee on One Health (2024–2025). Passionate about One Health, public health, and data analysis, she has spearheaded numerous antimicrobial resistance (AMR) projects, including public health awareness campaigns. Esther is a published writer, award-winning essayist, and advocate for interdisciplinary collaboration in health.