Tackling Antimicrobial Resistance: The Importance of Utilising the One Health Approach
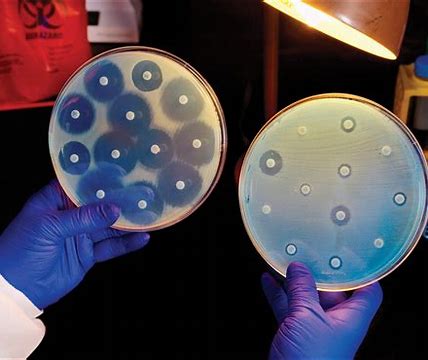

Thandizo Kapatsa
Thandizo Kapatsa is a Laboratory Technologist at Dedza District Hospital, holding a Bachelor of Science in Medical Microbiology from the Malawi University of Science and Technology. Thandizo is keenly interested in antimicrobial resistance, especially its behavioural aspects, the complex interactions between individuals and their environments and how this relates to their overall health. With her passions rooted in AMR, Thandizo aspires to pursue further education in antimicrobial stewardship to have an in-depth understanding and build expertise that can benefit public health and create opportunities for multidisciplinary partnerships with other professionals.